Cancer patients often ask their doctors, “What would you do if you were me?” Here, our Curious Dr. George (George Lundberg, MD) asks Mayo Clinic oncologist Sameer A. Parikh, MBBS, how he would handle his own diagnosis of chronic lymphocytic leukemia (CLL). Dr. Parikh is an Associate Professor of Medicine and Assistant Professor of Oncology at the Mayo Clinic in Rochester, Minnesota.
Curious Dr. George: Please imagine this hypothetical scenario: You are an active clinical and research oncologist in general good health. However, lately, you have felt less energy than usual, have been feeling fatigued at night, and have lost some weight without dieting. You decide to visit your primary care physician for a check-up. On physical examination, she notes that you are a little pale, and you have moderately enlarged lymph nodes in the axilla and groin, as well as a slightly enlarged liver and spleen. She orders several lab tests., which show that your hematocrit is 38, hemoglobin 12, WBCs 90 000 with mostly mature lymphocytes, and you have a proper number of granulocytes and normal platelets. You receive a provisional diagnosis of chronic lymphocytic leukemia. How would you proceed?
Sameer A. Parikh, MBBS: I chose to study leukemia because my maternal aunt passed away from acute myeloid leukemia at the age of 44, just three months after her diagnosis. Although chronic lymphocytic leukemia (CLL) is different, the word “leukemia” evokes feelings of helplessness and anxiety, making it difficult for anyone to process information properly. In your hypothetical scenario, although it would not be easy, I would make sure to collect my thoughts and give the diagnosis some time to process. I would also discuss the diagnosis with my close friends and family to garner all the support I would need as I navigate this period of uncertainty, with regard to outcomes following the diagnosis. I would then research the top experts in CLL and ensure I secure an appointment with a specialist. It’s crucial to consult with someone who specializes in CLL to obtain the most up-to-date information, as studies show that expertise-specific care leads to better outcomes.
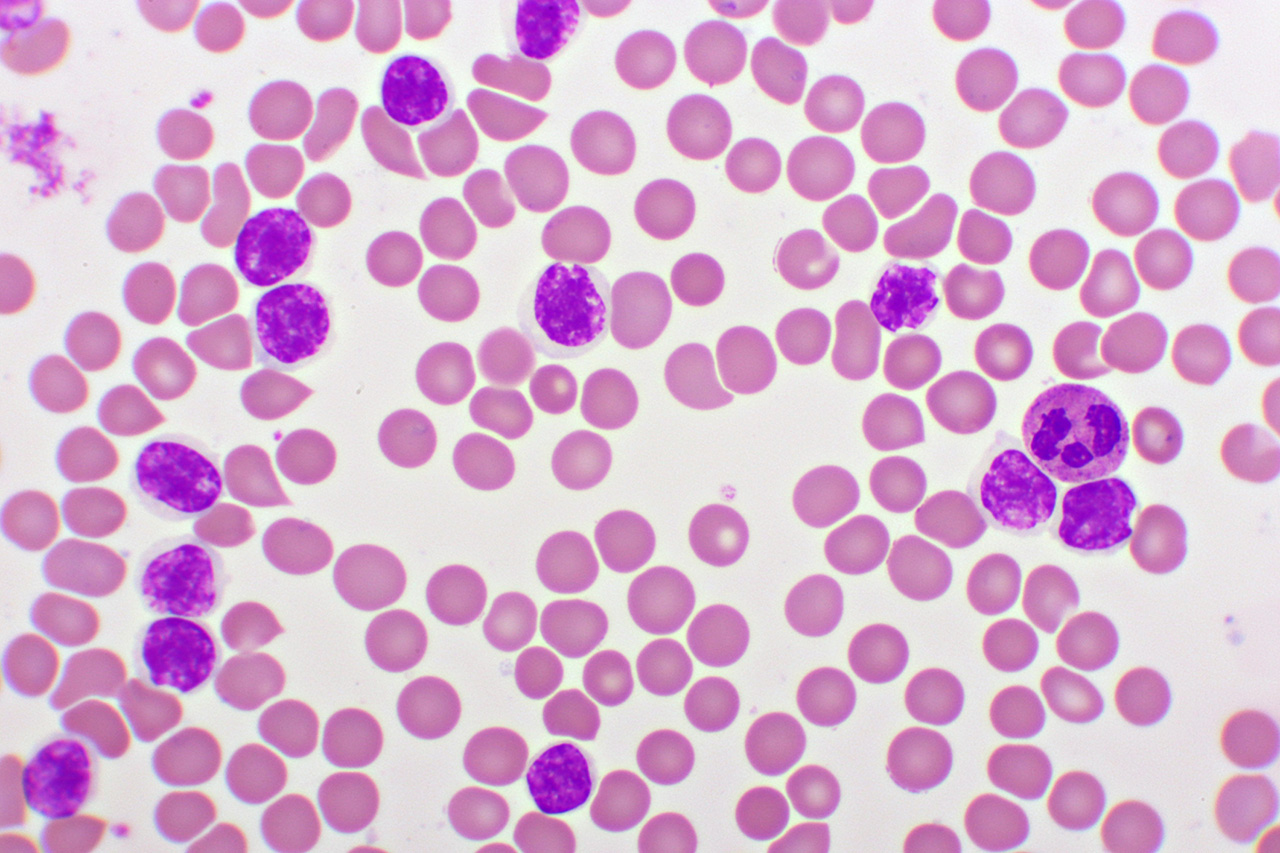
Confirming a diagnosis of CLL is extremely important, and it is typically done via a peripheral blood flow cytometry study. Unlike other malignancies, patients with early-stage, asymptomatic CLL are not treated at the time of initial diagnosis, unless a few specific, well-established criteria are met (as outlined in the 2018 guidelines of the International Workshop on Chronic Lymphocytic Leukemia, iwCLL2018). This is due to decades of research demonstrating that early intervention in CLL does not lead to improved quantity or quality of life. It is essential to understand this because it challenges the common belief of “find cancers early, so you can fix them early.”
In this imaginary case, although my WBC count is high, it appears that I would not need CLL-directed treatment at this time. One of the first questions I would have for my CLL specialist is how quickly my cancer is likely to progress to the point where treatment would be necessary. To better understand the biology of the underlying CLL, we would typically obtain several genetic tests, including IGHV mutation status, serum beta-2 microglobulin, TP53 mutation status, and the CLL FISH profile. The collection of these tests would allow us to calculate the CLL international prognostic index (CLL-IPI). Based on the total score, my CLL could be classified into low risk, intermediate risk, high risk, or very high risk of disease progression requiring treatment, with a 5-year need for therapy at 20%, 50%, 70%, and 90%, respectively for the corresponding CLL-IPI risk scores.
During this active surveillance, or the so called “watch and wait” phase of the disease process, it would be important to acknowledge the anxiety or emotional distress associated with untreated malignancy (“watch and worry”). Having the support of loved ones through this journey and acknowledging that treatment may be needed in the not-too-distant future would be exceedingly important, particularly given that there may be no external signs of cancer. In addition, it would also be important to see my primary care physician on a regular basis and stay up-to-date with cancer screening measures, including undergoing a colonoscopy and prostate cancer screening as recommended. Also, I would also schedule a yearly dermatology visit for a full-body skin check, given the increased risk of skin cancers in patients with CLL. Finally, I would follow the CDC recommendations for immunization in an immunocompromised host, and stay up to date with all the vaccinations.
Once treatment is needed, I would ensure to repeat the genomic tests to confirm that nothing has changed. Currently, there is no scenario in the management of CLL where chemotherapy is indicated. Instead, treatment consists of a fixed duration (12 to 24 months) of combination therapy with pills (either Bruton tyrosine kinase inhibitors or BCL2 inhibitors) and immunotherapy infusions (such as monoclonal antibody infusions like obinutuzumab). If these treatments stop working, newer options are available, including BTK degraders, bispecific antibodies, and chimeric antigen receptor (CAR-T) therapy, in addition to an allogeneic stem cell transplant.
While we would aim to cure my CLL with the treatments available, it would be important to remember that CLL remains an incurable disease and is managed as a chronic condition. I always remind my patients that this journey is a marathon, not a sprint, and we will grow old together. My goal as an oncologist, which would also hold true in my own case, is to ensure my patients reach their average life expectancy (and hopefully beyond that) without considering CLL with a high quality of life. With the tools we have at our disposal today, I am confident that we can achieve this objective for the majority of our patients.
Dr. Parikh can be reached at Parikh.Sameer@mayo.edu